Women face a disproportionate burden from autoimmune diseases, conditions in which the body’s immune system mistakenly attacks healthy tissues. Notably, researchers estimate that nearly 80% of individuals living with autoimmune disorders are female, underscoring a profound and persistent health disparity. Against this backdrop, this article examines the underlying reasons for this imbalance, explores common triggers, and outlines personalized management strategies that empower women to navigate their health more effectively. By gaining clarity and insight, women can take proactive steps toward improved well-being and quality of life.
Moreover, autoimmune diseases encompass more than 100 distinct conditions, ranging from relatively mild to life-altering in severity. As a result, they disrupt daily routines, cause chronic pain, and, in some cases, lead to irreversible organ damage. Nevertheless, early detection combined with tailored management plans can significantly transform outcomes, enabling many women to lead active and fulfilling lives.
The Prevalence of Autoimmune Diseases in Women
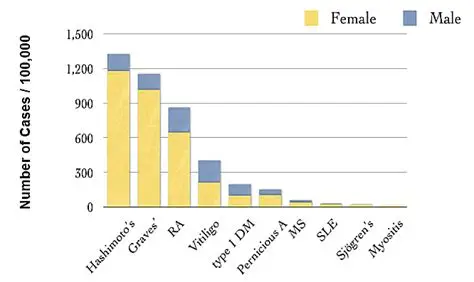
To begin with, statistics reveal a striking reality: autoimmune disorders affect women far more frequently than men. For example, conditions such as Sjögren’s syndrome occur nearly nine times more often in women. Researchers largely attribute this disparity to a complex interplay of biological, hormonal, and environmental factors that heighten vulnerability.
Additionally, incidence rates continue to rise both in the United States and globally. In particular, women in their reproductive years are more likely to receive diagnoses, a pattern that coincides with significant hormonal fluctuations. Consequently, this timing reinforces the urgent need for gender-specific research and awareness initiatives.
Furthermore, societal influences compound the problem. Women often delay seeking medical care, dismissing early symptoms as stress, exhaustion, or routine discomfort. Therefore, healthcare providers must adopt a more attentive and validating approach to bridge this diagnostic gap.
Common Autoimmune Diseases Affecting Women
Among the most prevalent conditions, lupus stands out prominently. Specifically, it triggers widespread inflammation, affecting joints, skin, kidneys, and the cardiovascular system. Alarmingly, women of color experience higher incidence and severity, adding layers of social and healthcare inequity.
Similarly, rheumatoid arthritis (RA) disproportionately impacts women. This condition leads to painful joint swelling, stiffness, and, if untreated, long-term deformities. Typically, symptoms are worse in the morning, significantly interfering with mobility and work productivity.
Meanwhile, multiple sclerosis (MS) affects the nervous system, causing fatigue, numbness, and vision impairment. Although women are often diagnosed earlier than men, disease progression varies considerably.
In addition, other notable autoimmune disorders include Hashimoto’s thyroiditis, which slows metabolism through thyroid destruction, and psoriasis, characterized by chronic inflammatory skin lesions. Collectively, these diseases share overlapping symptoms, often complicating diagnosis and delaying treatment.
Identifying Symptoms Early
Across many autoimmune conditions, fatigue emerges as a defining symptom. In many cases, women describe a profound exhaustion that does not improve with rest, signaling the need for further evaluation.
Alongside fatigue, joint pain and swelling frequently appear. Affected areas become tender and stiff, limiting daily function. Likewise, skin manifestations—such as rashes, dryness, or discoloration—serve as visible indicators, particularly in lupus and Sjögren’s syndrome.
Additionally, digestive disturbances, including abdominal pain and irregular bowel habits, may suggest gastrointestinal involvement. Recurrent fevers and swollen lymph nodes further complicate the picture, often mimicking infections. For this reason, symptom journaling becomes invaluable, helping clinicians identify patterns.
However, fluctuating symptoms pose diagnostic challenges. Blood tests measuring autoantibodies provide clarity. Ultimately, early intervention remains critical in preventing long-term complications.
Unraveling the Triggers
Autoimmune diseases often remain dormant until specific triggers activate them. Most commonly, infections—viral or bacterial—initiate immune misfires. For instance, certain viral exposures have been linked to lupus flares.
Beyond infections, environmental exposures significantly increase risk. Chemicals such as pesticides and industrial solvents correlate with higher incidence rates. In the case of lupus, sunlight exposure frequently exacerbates symptoms, necessitating protective measures.
Equally important, stress acts as a powerful catalyst. Remarkably, up to 80% of patients recall significant emotional stress before disease onset. Chronic stress weakens immune regulation, allowing autoimmunity to flourish.
Moreover, certain medications may provoke autoimmune reactions. Therefore, women must discuss complete medical histories with providers to minimize unintended triggers.
Genetic Factors at Play
Genetics establish the groundwork for susceptibility. Not surprisingly, family history significantly increases risk, with specific gene variants linked to RA, MS, and lupus.
Nevertheless, genetics alone rarely determine outcomes. Instead, genes interact dynamically with environmental exposures. Twin studies illustrate this clearly, as identical siblings do not always develop the same conditions.
Furthermore, women possess two X chromosomes, both carrying immune-related genes. This biological reality may partially explain higher prevalence, prompting ongoing research into preventive strategies.
The Role of Hormones
Hormonal fluctuations exert a profound influence on autoimmune activity. Notably, changes during puberty, pregnancy, and menopause often trigger symptom flares. For example, pregnancy may alleviate RA symptoms while worsening lupus.
Additionally, imbalances in progesterone and testosterone further disrupt immune regulation. As a result, hormonal therapies require careful supervision.
Meanwhile, menstrual cycles can intensify symptoms, making tracking essential. Consequently, endocrinologists and rheumatologists increasingly collaborate to design hormone-sensitive management plans.
Environmental and Lifestyle Influences
Daily environments shape autoimmune risk profiles. In particular, pollution and toxin exposure place constant stress on immune systems, especially in urban settings.
At the same time, diet represents a powerful, modifiable factor. Processed foods, gluten, and dairy provoke inflammation in susceptible individuals. Through elimination diets, women often identify and reduce triggers.
Equally, physical activity plays a protective role. While inactivity weakens resilience, moderate exercise strengthens immune balance. Thus, activities like walking or yoga strike an ideal balance.
Finally, smoking presents a clear and avoidable risk. It doubles RA risk and worsens pulmonary involvement in lupus. Encouragingly, cessation yields immediate health benefits.
Crafting Tailored Management Plans
Personalized care forms the foundation of effective autoimmune management. Rather than generic protocols, clinicians evaluate symptoms, medical histories, and lifestyle factors to design individualized plans.
Importantly, multidisciplinary teams enhance outcomes. Rheumatologists, nutritionists, mental health professionals, and physical therapists collaborate seamlessly. Through regular monitoring, plans evolve alongside patients’ needs.
Most importantly, patient participation drives success. Women actively contribute preferences and feedback, fostering ownership and adherence.
Medical Interventions
Pharmacological treatments suppress immune overactivity. Initially, NSAIDs alleviate pain and inflammation. For more severe cases, immunosuppressants such as methotrexate slow disease progression.
More recently, biologic therapies target specific inflammatory pathways, particularly in RA and MS. While effective, they require careful monitoring.
Meanwhile, corticosteroids offer rapid relief during flares but necessitate cautious tapering due to long-term risks.
Looking ahead, emerging therapies—including gene-based treatments and stem cell research—offer promising possibilities.
Lifestyle Modifications for Daily Wellness
Beyond medication, lifestyle changes empower women daily. Consistent sleep routines restore energy and reduce fatigue.
Similarly, low-impact exercise strengthens muscles and preserves joint function. When combined with pacing, activity becomes sustainable.
Additionally, social support buffers emotional strain. Support groups and online communities provide shared understanding and encouragement.
Stress Management Techniques
Managing stress remains indispensable. Practices such as meditation lower cortisol levels and improve immune balance.
Likewise, yoga integrates movement and mindfulness, easing both physical and emotional tension.
In moments of acute stress, deep breathing and journaling provide immediate relief. Furthermore, therapy—particularly cognitive behavioral approaches—helps women reframe challenges and build resilience.
Dietary Approaches to Reduce Inflammation
Nutrition plays a central role in disease control. Anti-inflammatory diets, rich in fruits, vegetables, and omega-3 fatty acids, reduce symptom severity.
Through elimination protocols, women identify sensitivities with precision.
Additionally, supplements such as vitamin D address common deficiencies. However, professional guidance remains essential.
Hydration supports cellular function and digestion. Thus, adequate water intake remains foundational.
Navigating Pregnancy with Autoimmunity
Pregnancy introduces unique considerations. While some conditions improve, others worsen, making preconception counseling vital.
Medication adjustments, close monitoring, and postpartum planning safeguard both mother and child.
Ultimately, individualized care ensures safe and informed decisions throughout this period.
The Future of Autoimmune Treatment
Looking forward, innovation reshapes care. Precision medicine, powered by genetics and AI, predicts flares and personalizes therapies.
Encouragingly, women-centered research expands clinical trial inclusivity. Advocacy efforts amplify voices, driving funding and policy reform.
Empowering Women Through Knowledge
In conclusion, women confront autoimmune diseases with strength, adaptability, and informed strategy. By identifying triggers, embracing tailored management plans, and integrating medical and lifestyle approaches, they move beyond survival toward thriving. As research advances, barriers continue to fall, promising healthier and more equitable futures for women worldwide.
