Introduction: Listening to a Quiet but Important Signal
Women’s bodies speak in subtle ways. Vaginal dryness, though often whispered about or silently endured, is one such signal—quiet, yet deeply impactful. Across cultures and generations, women have experienced it during different life stages. However, modern life, stress, hormonal shifts, and medical interventions have made it increasingly common.
Despite its prevalence, vaginal dryness remains misunderstood and under-discussed. Many women dismiss it as “normal” or feel hesitant to seek solutions. Yet, tradition teaches us that discomfort is never meant to be ignored. Forward-thinking healthcare echoes the same truth: vaginal dryness is manageable, treatable, and often reversible.
Understanding the condition is the first step. Acting with care and consistency is the next.
What Is Vaginal Dryness?
Vaginal dryness occurs when the vaginal tissues produce insufficient natural lubrication. As a result, the vaginal lining may feel tight, irritated, or inflamed. This dryness can affect daily comfort, intimacy, and emotional well-being.
While aging and menopause are commonly associated with the condition, they are not the only causes. Women of all ages may experience vaginal dryness at different points in their lives.
Rather than accepting discomfort as destiny, it is wiser to examine the underlying causes and address them thoughtfully.
Common Causes of Vaginal Dryness
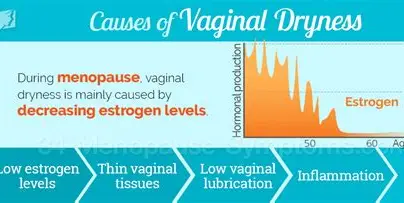
Hormonal Changes
Estrogen plays a vital role in maintaining vaginal moisture and elasticity. When estrogen levels decline, vaginal tissues become thinner and drier.
This hormonal shift may occur during:
- Menopause and perimenopause
- Breastfeeding
- Postpartum recovery
- Surgical removal of ovaries
Traditionally, women noticed these changes and adapted their routines accordingly. Modern medicine now helps us understand the biology behind them.
Stress and Lifestyle Factors
Chronic stress disrupts hormonal balance. Poor sleep, overwork, and emotional strain can quietly reduce vaginal lubrication.
Additionally, habits such as smoking and excessive alcohol consumption restrict blood flow and impair tissue health. Therefore, dryness may reflect not only physical changes but also lifestyle imbalances.
Medications and Medical Treatments
Certain medications interfere with natural lubrication, including:
- Antidepressants
- Antihistamines
- Hormonal contraceptives
- Chemotherapy and radiation therapy
While these treatments serve important purposes, their side effects deserve attention rather than silence.
Harsh Products and Hygiene Practices
Over-cleansing, scented soaps, and chemical washes disrupt the vagina’s natural pH. Ironically, products marketed for “intimate freshness” often worsen dryness.
Traditionally, women relied on simple cleansing with water. That wisdom still holds value today.
Symptoms Women Should Not Ignore
Vaginal dryness manifests differently for each woman. However, common symptoms include:
- Itching or burning sensations
- Pain or discomfort during intimacy
- Light spotting after intercourse
- Tightness or soreness
- Increased susceptibility to infections
These signs deserve respectful attention. Ignoring them often leads to worsening discomfort and emotional distress.
Why Addressing Vaginal Dryness Matters
Vaginal health is not separate from overall health. Discomfort affects confidence, relationships, and mental well-being. Moreover, untreated dryness increases the risk of infections and tissue injury.
From a skeptical standpoint, dismissing these symptoms as “just part of life” serves no one. Progress lies in informed care, not resignation.
How Lubricants Help
To begin with, lubricants offer fast and practical relief for vaginal dryness. They reduce friction, ease discomfort, and improve day-to-day comfort as well as intimacy. However, it is important to remember that not all lubricants are the same. Therefore, choosing the right one makes a meaningful difference.
Water-Based Lubricants
First and foremost, water-based lubricants are lightweight, non-greasy, and easy to wash off. Because of their gentle formulation, they work well for short-term relief. Additionally, they are safe to use with condoms, making them a common first choice for many women.
Pros:
- Gentle and widely available
- Safe for most women
Cons:
- May require frequent reapplication
As a result, these lubricants suit women who seek simple, short-term comfort without heaviness or residue.
Silicone-Based Lubricants
In contrast, silicone-based lubricants last significantly longer and provide a smoother, silkier feel. Since they do not absorb into the skin quickly, they are especially helpful for women experiencing moderate to severe dryness.
Pros:
- Long-lasting relief
- Excellent for intimacy
Cons:
- Harder to wash off
- Not compatible with silicone devices
From a practical perspective, these lubricants offer dependable comfort when dryness persists and frequent reapplication feels inconvenient.
Oil-Based Lubricants (With Caution)
Meanwhile, oil-based lubricants such as coconut oil have long-standing roots in traditional women’s care. While they can feel deeply soothing, they are not suitable for everyone and should be used with caution.
Caution:
- Can damage latex condoms
- May increase infection risk if not pure
Therefore, when used sparingly and mindfully, oil-based options may suit some women. Nevertheless, medical guidance is strongly advised before regular use.
Vaginal Moisturizers: Long-Term Support
Beyond immediate relief, vaginal moisturizers provide ongoing support. Unlike lubricants, they work gradually by restoring hydration to vaginal tissues over time.
When applied every few days, these products help maintain elasticity and daily comfort. Consequently, for women experiencing persistent dryness, moisturizers often deliver more consistent improvement.
In this case, consistency—rather than urgency—makes the true difference.
Hormonal Treatments: When Needed
However, when dryness becomes moderate to severe and is clearly linked to estrogen deficiency, lifestyle changes and over-the-counter products may not be enough. At this stage, medical treatments may be necessary.
Local Estrogen Therapy
Specifically, local estrogen therapy delivers estrogen directly to vaginal tissues through creams, tablets, or rings. This targeted approach improves tissue health without significantly affecting the rest of the body.
Benefits:
- Improves moisture and elasticity
- Minimal systemic absorption
As a result, this treatment aligns with modern medicine’s preference for effective yet low-risk solutions. Nevertheless, professional consultation remains essential before beginning any hormonal therapy.
Lifestyle Fixes That Truly Work
While products offer relief, lifestyle changes address root causes. These fixes require patience but yield lasting benefits.
Nourish the Body from Within
A balanced diet supports hormonal health. Foods rich in omega-3 fatty acids, such as flaxseeds and walnuts, improve tissue hydration.
Additionally, phytoestrogen-rich foods like soy, lentils, and chickpeas may help balance estrogen levels naturally.
Traditionally, women relied on nourishing meals rather than supplements. That principle still applies.
Stay Hydrated
Dehydration directly affects vaginal moisture. Drinking adequate water daily improves overall tissue hydration.
This simple habit is often overlooked, yet profoundly effective.
Reduce Stress Intentionally
Stress disrupts hormonal harmony. Practices such as yoga, meditation, and mindful breathing restore balance over time.
Ancient wellness systems emphasized calmness as medicine. Modern science now confirms their wisdom.
Choose Gentle Hygiene Practices
Avoid scented soaps, douches, and chemical cleansers. Clean the external area gently with lukewarm water.
Less intervention often leads to better balance.
Maintain Regular Intimacy
Healthy blood flow supports vaginal lubrication. Regular, comfortable intimacy—alone or with a partner—stimulates tissue health.
However, pressure-free intimacy matters more than frequency.
When to See a Doctor
Self-care helps many women. Nevertheless, medical advice becomes necessary if:
- Dryness persists despite home remedies
- Pain worsens
- Recurrent infections occur
- Bleeding appears
Seeking help reflects strength, not weakness.
Emotional Well-Being and Vaginal Health
Vaginal dryness often affects self-esteem and relationships. Open communication with partners fosters understanding and emotional closeness.
Silence, by contrast, deepens discomfort. Tradition teaches us that shared burdens lighten with compassion.
Myths Around Vaginal Dryness
“It Only Happens After Menopause”
False. Women of all ages experience it.
“It Is Something to Be Endured”
False. Solutions exist and work.
“Lubricants Are Unnatural”
False. Thoughtfully chosen products support natural comfort.
Questioning myths leads to empowerment.
The Future of Women’s Intimate Health
Research in women’s health continues to expand. New formulations, hormone-free treatments, and personalized care approaches promise improved comfort.
Yet, progress must remain grounded in respect for women’s experiences—not rushed commercialization.
The future lies in blending traditional wisdom with scientific clarity.
Conclusion: Comfort Is a Right, Not a Luxury
Vaginal dryness may be common, but it should never be ignored. It is the body’s way of asking for attention, balance, and care.
Through informed choices—whether lubricants, moisturizers, lifestyle changes, or medical support—women can reclaim comfort and confidence.
Honoring the body, listening without judgment, and responding with patience form the true solution. In doing so, women not only heal discomfort but also reaffirm a timeless truth: well-being is foundational, and every woman deserves it.
Vaginal health:
https://shebreaksbarriers.org/wp-admin/post.php?post=251&action=edit