Get the most current information on Breast Implant Illness (BII) symptoms, including fatigue and brain fog, and learn the essential steps to take before and after breast augmentation surgery.
For decades, breast implants have been a choice for millions of women—whether for reconstruction after mastectomy or for cosmetic augmentation. It is a deeply personal decision rooted in self-image, healing, and confidence. Yet, in recent years, a crucial and often confusing conversation has emerged: Breast Implant Illness (BII).
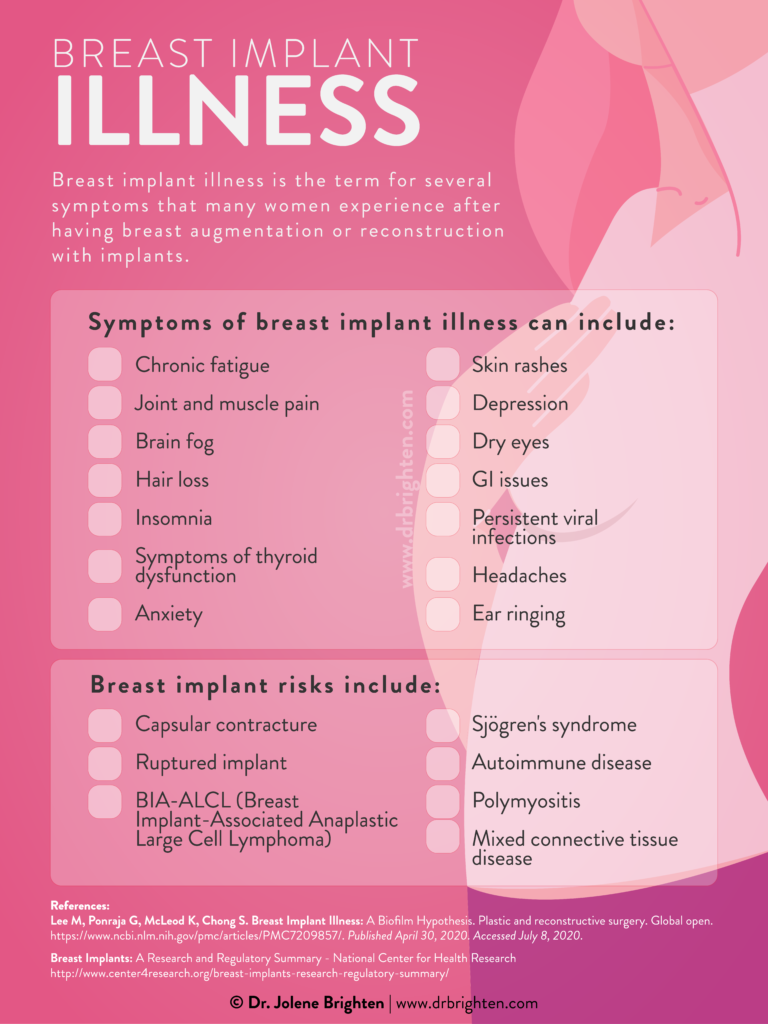
BII is the term used to describe a collection of systemic symptoms that some women experience with both silicone and saline implants. While it currently lacks a single, official medical diagnosis code, the collective experiences of tens of thousands of women have made it a widely recognized phenomenon by patients, advocates, and a growing number of medical professionals. The latest data and reports confirm BII is a legitimate, complex health concern.
The purpose of this article is not to frighten, but to empower you with knowledge—the kind that allows you to make informed decisions and advocate fiercely for your health, whether you are considering surgery or you are years post-op.
The Most Commonly Reported Symptoms of BII in 2025
Breast Implant Illness is often described as a “Systemic Illness,” meaning it affects the entire body, not just the breast area. Because BII symptoms can mimic those of other autoimmune conditions, diagnosis is often a process of exclusion, ruling out thyroid issues, chronic fatigue syndrome, or rheumatological disorders first.
Symptoms can appear immediately after surgery or years later (the average reported time is around 5.4 years).
Here are the most frequently reported symptoms, based on patient reports submitted to regulatory bodies like the FDA and recent medical literature:
1. Systemic & Neurological Symptoms (The Most Prevalent)
These symptoms often impact daily function and are the most common complaint among women with BII:
Chronic Fatigue: Profound, debilitating tiredness that is not relieved by rest or sleep.
“Brain Fog”: Cognitive dysfunction, including difficulty concentrating, memory loss, mental confusion, and trouble finding words.
Anxiety & Depression: New or worsened anxiety, unexplained panic attacks, or persistent feelings of hopelessness and low mood.
Sleep Disturbances: Persistent insomnia or unrefreshing sleep.
2. Musculoskeletal Symptoms (Pain & Stiffness)
Joint Pain (Arthralgia) & Stiffness: Aching, pain, or stiffness in joints (knees, hips, hands) that often feels like arthritis but may not respond to standard treatments.
Muscle Aches (Myalgia) & Weakness: Widespread, unexplained muscle pain and a feeling of general weakness or heaviness in the limbs.
Fibromyalgia-like Symptoms: Many BII patients report symptoms that meet the criteria for Fibromyalgia, including tenderness and chronic, widespread pain.
3. Immunological & Inflammatory Symptoms
BII is often theorized to be an autoimmune or inflammatory response to the implant shell or filling material (silicone).
Signs of Autoimmunity: Developing or testing positive for autoimmune conditions (like Lupus, Rheumatoid Arthritis, or Sjogren’s syndrome).
Hair Loss: Unexplained, persistent shedding or thinning of hair.
Skin Issues: Rashes, dryness, itching, or new sensitivities.
Dry Eyes and Mouth: Chronic dryness that often suggests an inflammatory or autoimmune process.
Swollen Lymph Nodes: Tenderness or persistent swelling in the lymph nodes, especially in the armpit (axilla) or neck.
4. Local Breast Symptoms (While not always BII, they often accompany it)
Capsular Contracture: The hardening and tightening of the scar tissue (capsule) around the implant, causing pain, firmness, and distortion of the breast shape.
Breast Pain: Persistent discomfort, aching, or burning sensations in the breast tissue.(Source: FDA Medical Device Reports, patient-reported data, and systematic reviews of BII literature, 2024-2025)
Before Surgery: What Every Woman Must Ask
If you are considering breast augmentation or reconstruction, you must be your own strongest advocate. This is not just a cosmetic decision; it is a major medical procedure.
1. Know Your Risk Factors
While BII can affect anyone, studies suggest certain individuals may be more susceptible. Be honest with your surgeon about:
Personal or Family History of Autoimmunity: Lupus, Multiple Sclerosis, Rheumatoid Arthritis, etc.
Chronic Inflammatory Conditions: History of severe allergies, Irritable Bowel Syndrome (IBS), Chronic Fatigue Syndrome (CFS), or Fibromyalgia.
Chemical Sensitivity: Known extreme sensitivity to chemicals or metals.
If you have these risk factors, a surgeon experienced in BII should guide you through alternative options, like fat grafting (using your own body fat for augmentation), or offer a more cautious approach.
2. Understand the Implant Details
Don’t just choose size. Ask these essential questions about the devices:
Saline vs. Silicone: BII is reported with both types.
Textured vs. Smooth: Textured implants have a different, albeit rare, cancer risk (BIA-ALCL, which is separate from BII but equally important).
Component Disclosure: Ask for the detailed product insert that lists all materials used in the shell, fill, and even trace chemicals.
3. Plan for Maintenance and Removal
Implants are not lifetime devices. They have a lifespan and may need replacement or removal.
Screening: Silicone implants require routine imaging (usually MRI) to screen for silent ruptures, as recommended by the FDA.
Explantation Protocol: Ask your surgeon if they are experienced in Explantation (implant removal) with Total Capsulectomy (removing the implant plus the entire surrounding scar capsule). This is the gold standard for BII treatment.
After Surgery: A Proactive Health Checklist
If you currently have implants, whether you feel symptomatic or not, adopting a proactive health approach is crucial.
1. Monitor Systemic Health
Symptom Journal: Maintain a detailed log of any new, chronic, or worsening symptoms, especially fatigue, brain fog, and joint pain. Note when they start and how long they last.
Holistic Bloodwork: If you feel unwell, ask your primary care provider to test for common rule-outs like thyroid disease, Lyme disease, and basic autoimmune markers (ANA, CRP, ESR).
2. Address Inflammation Daily
The leading theory for BII involves chronic inflammation. You can manage this with lifestyle:
Nutrition: Focus on an anti-inflammatory diet rich in whole foods, quality proteins, and healthy fats (Omega-3s). Reduce processed foods, sugar, and known food sensitivities.
Toxin Reduction: Minimize exposure to environmental toxins found in cleaning products, plastics, and personal care products to ease the burden on your body’s detoxification systems.
3. Trust Your Instincts and Seek Specialized Care
If you are experiencing symptoms and your doctor dismisses them, get a second opinion. Find a healthcare provider—a plastic surgeon, a functional medicine doctor, or a rheumatologist—who acknowledges BII and is willing to work with you on an elimination and treatment plan.
The single most effective reported treatment for BII is the surgical explantation with total capsulectomy. Numerous patient reports and studies show a significant improvement in systemic symptoms after the implants and the surrounding capsule are removed.
You are the expert on your own body. This journey may be challenging, but with knowledge and self-advocacy, you can navigate it with strength and grace, and ultimately reclaim your wellness.Would you like me to suggest some alternative titles for this article?