Women grow stronger when they understand their bodies and respond with wisdom rather than fear. Uterine fibroids, common non-cancerous growths of the uterus, affect millions of women worldwide. Yet, despite their prevalence, they often remain unnoticed until they begin to disrupt daily life.
This in-depth guide explains uterine fibroid symptoms in women, underscores the importance of early detection, and outlines effective non-surgical treatment options. With awareness and timely action, women can preserve fertility, protect long-term health, and live with renewed confidence.
What Are Uterine Fibroids?
Uterine fibroids—clinically known as leiomyomas or myomas—originate from the smooth muscle tissue of the uterus. Their size varies dramatically, from tiny seed-like nodules to large masses capable of distorting the uterine structure.
Most women develop fibroids during their reproductive years, particularly between ages 30 and 50. Hormones such as estrogen and progesterone significantly influence their growth, while genetics and lifestyle factors, including obesity, further increase risk.
Importantly, fibroids often shrink after menopause as hormone levels decline. Moreover, they rarely become cancerous, a fact confirmed by leading medical institutions such as the Mayo Clinic.
🔗 https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/symptoms-causes/syc-20354288
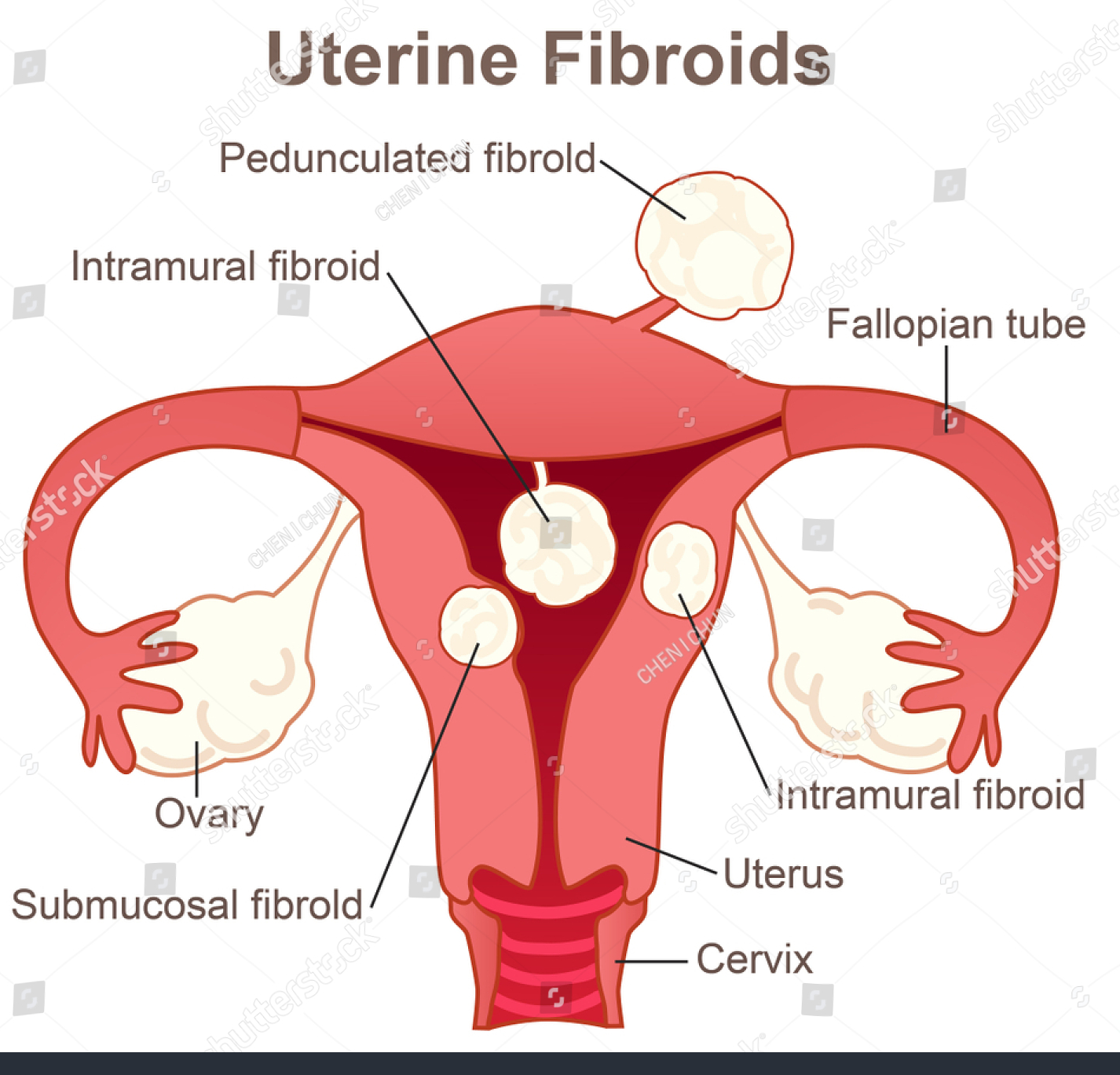
Fibroids are classified by location:
- Submucosal fibroids (inside the uterine cavity) – often cause heavy bleeding
- Intramural fibroids (within the uterine wall) – the most common type
- Subserosal fibroids (on the outer surface) – typically cause pressure symptoms
Understanding these types allows women to communicate more effectively with healthcare providers.
🔗 https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
Common Symptoms of Uterine Fibroids in Women
One of the earliest warning signs is heavy or prolonged menstrual bleeding. Periods may last longer than seven days, include large clots, and require frequent changes of sanitary products—disrupting work, rest, and emotional well-being.
In addition, many women experience pelvic pain or pressure, often described as a sensation of fullness in the lower abdomen. Menstrual cramps may worsen, while pain can radiate to the lower back or legs, sometimes resembling endometriosis.
As fibroids enlarge, they may press on surrounding organs:
- Frequent urination, particularly at night, due to bladder compression
- Constipation or difficulty emptying the bowel when pressure affects the rectum
Furthermore, some women experience pain during sexual intercourse (dyspareunia), which may strain intimate relationships. A visibly enlarged abdomen can also affect body image and self-esteem.
Chronic heavy bleeding frequently leads to iron-deficiency anemia, resulting in fatigue, dizziness, shortness of breath, and weakness.
🔗 https://www.webmd.com/women/uterine-fibroids/uterine-fibroids-anemia
In certain cases, fibroids interfere with fertility by blocking fallopian tubes or altering the uterine cavity. During pregnancy, they may increase the risk of miscarriage, preterm labor, or abnormal fetal positioning. Still, it is worth noting that 20–50% of women with fibroids experience no symptoms at all, discovering them during routine examinations.
Why Early Detection of Fibroids Is Essential
Early detection acts as a quiet safeguard against future complications. When fibroids remain untreated, symptoms often intensify, leading to chronic pain, severe anemia, or reproductive challenges.
More importantly, diagnosing fibroids early expands access to non-surgical management options. Delayed detection may limit choices and increase the likelihood of invasive procedures, including hysterectomy.
For women planning families, early intervention preserves fertility and protects uterine health. In this sense, knowledge is not merely power—it is prevention.
How Uterine Fibroids Are Diagnosed
Routine gynecological examinations serve as the first line of detection. During a pelvic exam, a physician may notice an enlarged or irregularly shaped uterus.
To confirm the diagnosis, doctors may recommend imaging tests such as:
- Transvaginal ultrasound – the most commonly used diagnostic tool
- MRI scans – provide detailed mapping of fibroid size and location
- Sonohysterography – improves detection of fibroids within the uterine cavity
Blood tests help identify anemia caused by excessive bleeding, while hysteroscopy allows direct visualization of the uterus when needed.
🔗 https://www.acog.org/womens-health/faqs/uterine-fibroids
Equally vital is self-awareness. Tracking menstrual cycles and symptoms encourages earlier medical consultation and timely care.
Non-Surgical Treatment Options for Uterine Fibroids
Fortunately, many women manage fibroids effectively without surgery.
Hormonal therapies, including birth control pills and progestin-releasing IUDs, help regulate menstrual bleeding and reduce pain.
🔗 https://www.plannedparenthood.org/learn/health-and-wellness/uterine-fibroids
GnRH agonists temporarily shrink fibroids by lowering estrogen levels, though they are typically prescribed for short-term use due to menopausal-like side effects.
For women seeking non-hormonal relief, tranexamic acid reduces heavy menstrual bleeding, while NSAIDs such as ibuprofen alleviate pain and inflammation.
Minimally invasive procedures include:
- Uterine artery embolization (UAE) – blocks blood flow to fibroids
- MRI-guided focused ultrasound – uses sound waves to destroy fibroid tissue without incisions
Lifestyle Changes That Support Relief
Diet and lifestyle choices play a supportive role in fibroid management. Anti-inflammatory foods—fruits, vegetables, whole grains—help regulate hormones, while limiting red meat and processed dairy may slow fibroid growth.
Maintaining a healthy weight, engaging in regular physical activity, and managing stress through yoga or meditation contribute to hormonal balance. Some studies suggest vitamin D deficiency may be linked to fibroids.
Complementary therapies such as acupuncture and heat therapy offer additional comfort for pelvic pain, while adequate hydration and sleep restore overall vitality.
When to See a Doctor
Medical attention is essential if symptoms interfere with daily life. Seek immediate care for:
- Bleeding that soaks pads hourly
- Persistent pelvic pain or sudden sharp abdominal pain
- Severe fatigue or breathlessness from anemia
- Difficulty conceiving
Regular annual check-ups remain the cornerstone of early detection and personalized care.
Empowerment Through Awareness
True empowerment begins with education. When women understand uterine fibroids, fear gives way to informed decision-making. Asking questions, exploring treatment options, and advocating for one’s health ensures care aligns with personal goals—whether symptom control or fertility preservation.
In conclusion, while uterine fibroids pose challenges, early detection and non-surgical relief options offer hope and control. Listen to your body. Seek knowledge. Act early. Your well-being is both your heritage and your responsibility—worth guarding with care and courage.