Pain stands among the most universal human experiences, yet it rarely unfolds in a uniform way. Although pain may appear to be a straightforward biological response to injury or illness, scientific research reveals a far more intricate reality. Men and women experience pain differently in intensity, duration, triggers, and even in how healthcare systems perceive and treat it. Recognizing these differences moves beyond academic curiosity; it directly shapes health equity, clinical precision, and compassionate medical care.
For decades, medical research relied primarily on male bodies as the standard biological model. As a result, clinicians frequently misunderstood, minimized, or misattributed women’s pain. Today, however, a growing body of research demonstrates that women experience pain through a complex interaction of biological mechanisms, hormonal fluctuations, genetic factors, psychological influences, and social conditioning. By examining these layers carefully, researchers and clinicians can better understand why women experience pain differently than men—and why healthcare systems must evolve to meet these distinct needs.
Understanding Pain: More Than a Physical Sensation
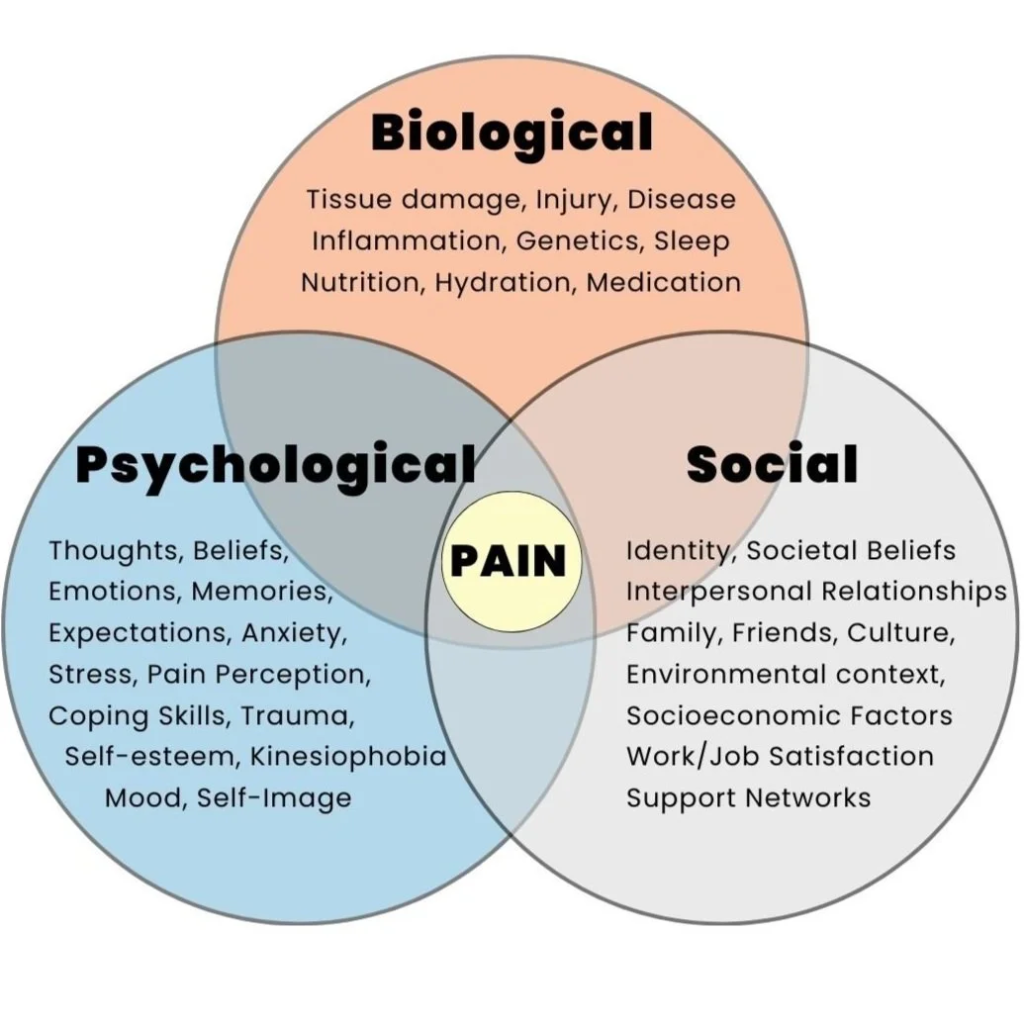
Pain does not function as a simple signal traveling from injured tissue to the brain. Instead, the nervous system, emotional state, prior experiences, and cultural context collectively shape the pain experience. The brain actively interprets pain signals, assigns meaning to them, and determines their intensity and emotional impact.
Importantly, this process does not operate identically in all individuals. Biological sex directly influences how the nervous system transmits, amplifies, or suppresses pain signals. At the same time, gender roles and social expectations shape how individuals express, tolerate, and seek treatment for pain. Therefore, any meaningful discussion of pain differences between women and men must consider both biological sex and social experience.
Biological Differences in Pain Processing
At a fundamental level, women and men differ biologically, and these differences significantly influence pain perception. Research consistently shows that women report pain more frequently and often describe it as more intense or longer lasting than men. This pattern appears across a wide range of conditions, including migraines, arthritis, fibromyalgia, irritable bowel syndrome, and autoimmune disorders.
The nervous system itself partly explains these differences. Studies suggest that women may possess a higher density of nerve fibers involved in pain transmission. Additionally, sex-specific variations in spinal cord and brain pain pathways alter how the body processes and perceives painful stimuli.
Moreover, inflammation—a major contributor to pain—often behaves differently in female bodies. Women’s immune systems tend to produce stronger inflammatory responses, which can heighten pain sensitivity, particularly in chronic inflammatory conditions.
The Powerful Role of Hormones
Hormones play a central role in shaping how women experience pain. Estrogen, progesterone, and other reproductive hormones actively influence pain sensitivity throughout a woman’s life. Unlike men, whose hormone levels remain relatively stable, women undergo cyclical hormonal changes during menstruation, pregnancy, and menopause.
Estrogen, in particular, can either amplify or reduce pain depending on its concentration and timing. During certain phases of the menstrual cycle, lower estrogen levels often increase pain sensitivity. This fluctuation helps explain why many women report worsening migraines, pelvic pain, or joint discomfort at specific times of the month.
Pregnancy introduces another significant hormonal shift. While increased endorphin levels reduce pain sensitivity for some women, others experience heightened discomfort due to musculoskeletal strain and nerve compression. Later in life, menopause brings declining estrogen levels, which often coincide with joint pain, headaches, and increased vulnerability to chronic pain disorders.
Thus, women’s pain does not remain static; it evolves alongside hormonal changes across the lifespan.
Genetic Influences on Pain Sensitivity
Genetic factors also shape pain perception. Certain genes involved in pain modulation and neurotransmitter activity express differently in women and men. These genetic variations influence both the strength of pain signal transmission and the body’s ability to regulate or suppress pain.
Furthermore, women show greater susceptibility to conditions associated with altered pain processing, such as fibromyalgia and chronic fatigue syndrome. These disorders involve central sensitization, a state in which the nervous system becomes excessively responsive to stimuli. Genetic predisposition, combined with hormonal and immune influences, increases the likelihood of such conditions in women.
Chronic Pain Conditions Are More Common in Women
One of the most striking differences between men and women appears in the prevalence of chronic pain conditions. Women disproportionately experience disorders marked by persistent or recurrent pain.
Conditions such as migraines, temporomandibular joint disorders, endometriosis, interstitial cystitis, and autoimmune diseases occur far more frequently in women. These illnesses often arise from complex interactions among the nervous system, immune responses, and hormonal regulation.
Endometriosis, for example, affects millions of women worldwide and causes severe pelvic pain. Despite its prevalence, clinicians frequently underdiagnose the condition. Many women wait years for an accurate diagnosis, which highlights how healthcare systems often overlook or normalize women’s pain.
Psychological and Emotional Dimensions of Pain
Pain does not exist independently of the mind. Emotional health strongly influences how individuals perceive and endure pain. Women experience anxiety and depression at higher rates than men, and these conditions can intensify pain perception.
In addition, women often manage multiple social roles—as caregivers, professionals, and family anchors—which increases stress levels. Chronic stress sensitizes the nervous system and lowers pain thresholds, thereby magnifying physical discomfort.
Importantly, this relationship does not suggest that women’s pain is imaginary or purely psychological. Instead, it reinforces the understanding that pain is a biopsychosocial phenomenon shaped by both physiological and emotional factors.
Social Conditioning and Gender Expectations
Beyond biology, social conditioning powerfully shapes pain experiences. From early childhood, society teaches boys and girls different lessons about pain. Boys often learn to suppress pain and display toughness, whereas girls receive greater permission to express discomfort.
These expectations influence how individuals report pain and how others interpret it. Men may underreport pain due to social pressure, while women often describe their pain more openly. Unfortunately, this openness sometimes disadvantages women in clinical environments.
Research shows that clinicians more frequently dismiss women’s pain complaints, attribute them to emotional causes, or label them as exaggerated. In contrast, clinicians often investigate men’s pain more promptly and treat it more aggressively. This gender bias contributes to delayed diagnoses and inadequate pain management for women.
The Medical System and Gender Bias in Pain Treatment
Historically, medicine underestimated women’s pain. For many years, researchers excluded women from clinical trials due to concerns about hormonal variability. Consequently, scientists tested numerous pain medications primarily on male subjects, creating significant gaps in understanding how these treatments affect women.
Even today, evidence suggests that healthcare providers offer women less adequate pain relief in emergency settings. Clinicians more often prescribe sedatives or antidepressants rather than pain-specific medications. These practices reflect persistent stereotypes that frame women as emotionally distressed rather than physically ill.
Correcting this imbalance requires systemic change, including inclusive research practices, improved medical education, and a commitment to listening to women’s experiences without prejudice.
Pain Communication: Different Languages of Suffering
Women and men often communicate pain differently. Women tend to describe pain in detailed and emotionally nuanced language, while men often present pain in brief, functional terms. These differences influence how clinicians interpret symptoms.
Although clinicians sometimes misinterpret detailed descriptions as exaggeration, such narratives often provide crucial diagnostic information. When healthcare professionals recognize and respect diverse communication styles, they improve diagnostic accuracy and deliver more empathetic care.
The Impact of Reproductive Health on Pain Experience
Women’s reproductive biology introduces pain experiences that men do not encounter. Menstrual cramps, ovulation pain, pregnancy-related discomfort, childbirth, and postpartum recovery impose significant physical demands on the body.
Despite their frequency, healthcare systems often dismiss these experiences as “normal.” While these forms of pain may be common, they still require appropriate attention and care. Normalizing pain should never justify neglecting it.
Toward Better Pain Care for Women
Understanding why women experience pain differently marks only the beginning. Healthcare systems must now translate this knowledge into action. Researchers and clinicians need to adopt sex-specific research frameworks and develop pain management strategies that reflect women’s unique biological realities.
Equally important, society must cultivate a culture of belief and respect. When women report pain, healthcare providers must listen carefully, validate their experiences, and respond with seriousness. Education within medical institutions and public discourse plays a crucial role in dismantling harmful stereotypes.
Looking Ahead: A More Inclusive Future
Pain research is moving steadily toward personalization. Advances in neuroscience, genetics, and endocrinology promise more tailored and effective pain management approaches. By acknowledging sex-based differences rather than ignoring them, medicine can become both more precise and more humane.
Women’s pain does not represent a deviation from the norm; it constitutes a vital dimension of human health. When science listens attentively, it not only reduces suffering but also restores dignity.
Conclusion
Women experience pain differently than men due to a complex interplay of biological, hormonal, genetic, psychological, and social factors. These differences shape not only how pain manifests but also how healthcare systems respond to it—often inadequately. For generations, medical science placed women’s pain at the margins of understanding. Today, however, research offers a clear opportunity to correct this imbalance.
By embracing a nuanced and inclusive understanding of pain, healthcare systems can move closer to equity, accuracy, and compassion. In doing so, they affirm a fundamental truth: pain deserves understanding, not dismissal—and every voice deserves to be heard.
Gender bias healthcare:
https://shebreaksbarriers.org/wp-admin/post.php?post=426&action=edit
