Women enter their 40s carrying earned wisdom, emotional depth, and the quiet authority of lived experience. However, this chapter of life often ushers in subtle physiological shifts—particularly in vaginal health—shaped by perimenopause and menopause. As a result, dryness, irritation, or gentle changes in intimacy may surface. Are these changes unsettling? At times, yes. Yet are they manageable? Most certainly.
With that in mind, informed care and respectful attention to the body’s signals become essential. When approached thoughtfully, comfort and confidence need not diminish with age. Instead, they can evolve. Accordingly, this guide offers practical, evidence-based strategies to help you navigate midlife vaginal health with grace, resilience, and quiet assurance.
Understanding Vaginal Changes After 40
As estrogen levels fluctuate and gradually decline, vaginal tissues may become thinner, less elastic, and drier—a condition clinically known as genitourinary syndrome of menopause (GSM). Studies suggest that nearly half of women experience symptoms such as dryness or discomfort within a few years after menopause.
These hormonal shifts may also increase susceptibility to urinary tract infections (UTIs) and yeast imbalance. Burning, itching, recurrent infections, or pain during intercourse are not mere inconveniences; they are signals worth honoring.
Daily Hygiene Habits That Support Vaginal Health
Time-honored simplicity remains best. Gentle daily care protects the vagina’s natural ecosystem.
- Choose breathable cotton underwear to minimize moisture and irritation
- Cleanse externally with lukewarm water and mild, fragrance-free soap
- Avoid douching or scented products that disrupt vaginal pH
- Pat dry—never rub—to preserve delicate skin integrity
Annual gynecological visits are not merely routine; they are acts of preventive wisdom.
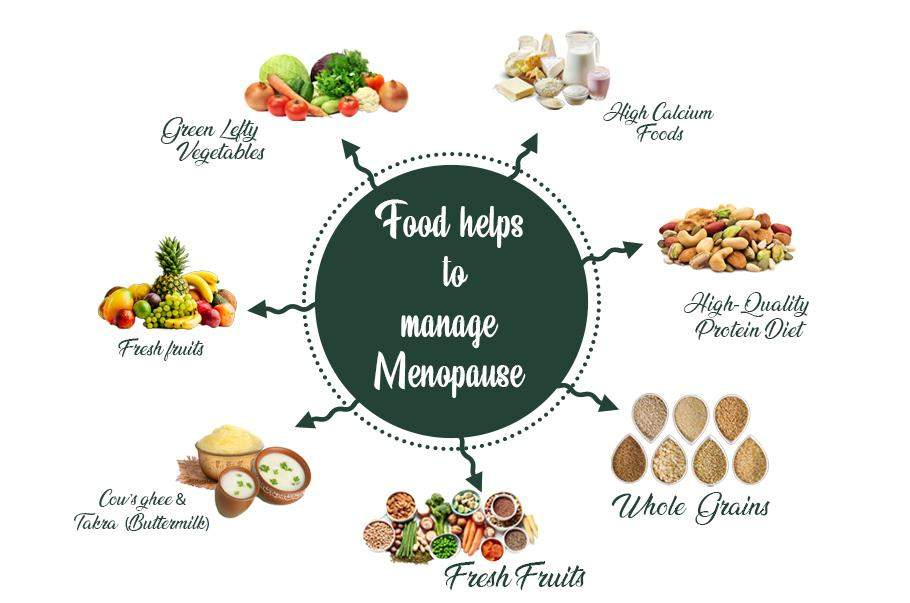
Nourishing Vaginal Health from Within
The body often heals best when nourished steadily and patiently.
A Mediterranean-style diet—rich in vegetables, fruits, whole grains, legumes, nuts, and olive oil—supports hormonal balance and tissue health. Foods containing phytoestrogens, such as soy, flaxseeds, and lentils, may gently ease dryness by mimicking estrogen’s effects.
Hydration remains fundamental. Adequate water intake sustains mucosal moisture throughout the body, including vaginal tissues. Limiting caffeine, alcohol, and overly spicy foods can further reduce irritation and vasomotor symptoms.
👉 Recommended reading:
Mediterranean-style diet guide :
🔗 https://www.health.harvard.edu/staying-healthy/the-mediterranean-diet
Strengthening the Pelvic Floor: A Timeless Practice
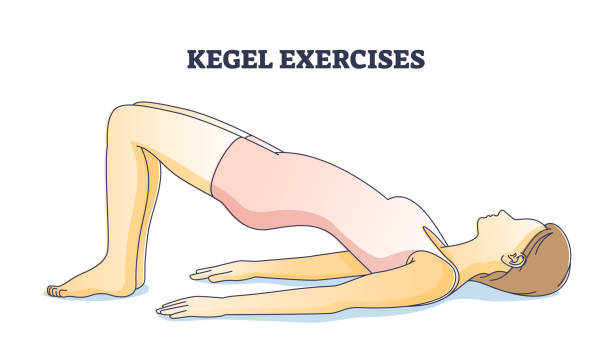
Pelvic floor health has been emphasized for generations—and rightly so. Strong, flexible muscles improve circulation, bladder control, and sexual satisfaction.
Kegel exercises, when performed consistently, enhance vaginal tone and resilience. Complement them with functional movements such as squats or bridges, and counterbalance tension with restorative poses like child’s pose.
If uncertainty arises, pelvic floor physiotherapy offers expert guidance tailored to individual needs.
pelvic floor physiotherapy visit 🔗 https://my.clevelandclinic.org/health/treatments/14459-pelvic-floor-physical-therapy
Intimacy After 40: Comfort Without Compromise
Intimacy evolves—it does not expire. Regular sexual activity, whether partnered or solo, promotes blood flow and natural lubrication. Extended foreplay and open communication allow arousal to build gradually, honoring the body’s changing rhythms.
Water-based lubricants reduce friction, while vaginal moisturizers used several times weekly support ongoing hydration. Comfort fosters confidence; confidence rekindles desire.
Natural and Medical Support Options
Non-hormonal solutions such as hyaluronic acid vaginal moisturizers offer effective hydration. Natural oils may provide lubrication, though they should not be used with latex condoms.
Low-dose vaginal estrogen therapy, prescribed by a healthcare professional, remains one of the most effective treatments for persistent GSM symptoms, with minimal systemic absorption.
The question is not whether help exists—but whether one gives herself permission to seek it.
When to Seek Medical Guidance
Persistent pain, post-coital bleeding, recurrent infections, or unusual discharge warrant professional evaluation. Early intervention preserves comfort and prevents complications.
Specialists such as urogynecologists or pelvic floor therapists provide targeted care rooted in both modern science and clinical tradition.
Emotional Confidence and Midlife Self-Respect
The body and mind move in concert. Hormonal changes may influence mood, sleep, and self-image. Mindfulness practices, journaling, and meaningful social connections foster emotional steadiness.
Midlife is not a diminishment—it is a distillation. Confidence grows when one treats herself with patience rather than criticism.
Embracing Midlife with Strength and Grace
Vaginal health after 40 is not about reclaiming youth—it is about honoring continuity. With informed habits, respectful care, and professional guidance when needed, comfort and vitality remain well within reach.
Every woman’s journey is singular. Listen carefully. Act thoughtfully. And step forward with the quiet confidence that comes from knowing your body—and valuing it.
👉 Supportive read: Mental Well-Being During Menopause https://shebreaksbarriers.org/wp-admin/post.php?post=110&action=edit
