Feeling dryness, burning, or pain? Learn about effective vaginal atrophy exercises and natural remedies to restore moisture, elasticity, and comfort after menopause.
Menopause is a massive transition, marking not just the end of menstruation, but the beginning of a whole new phase of life. It’s a time of newfound freedom for many, but it can also bring deeply uncomfortable changes that women often feel too awkward or ashamed to discuss.
If you are experiencing vaginal dryness, burning, itching, or pain during intercourse, you are not alone. These are often the hallmark signs of Vaginal Atrophy, also known as Genitourinary Syndrome of Menopause (GSM).
Let’s be clear: this is not a sign of aging “failure.” It is a completely normal, physiological response to the drop in hormones. And the most important thing to know is that you absolutely do not have to live with the discomfort. We’re going to discuss exercises and simple natural remedies you can use to restore comfort, elasticity, and intimacy.
Understanding the Change: What is Vaginal Atrophy (GSM)?
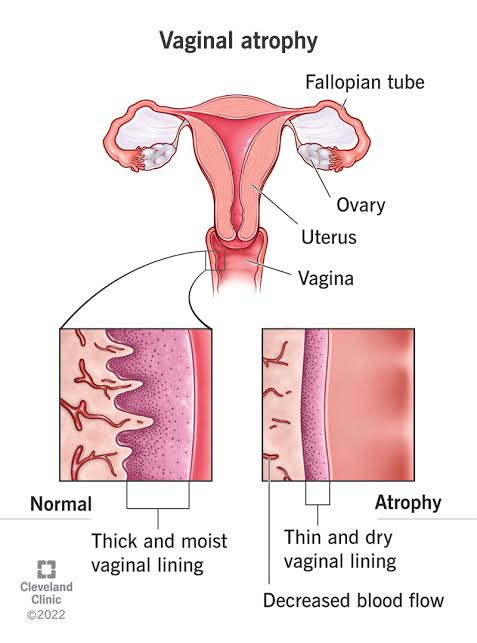
Vaginal Atrophy is caused by the precipitous drop in estrogen that occurs during and after menopause. Estrogen is the hormone that kept the vaginal and vulvar tissues plump, moist, and elastic.
When estrogen levels fall, the tissues change:
•Thinning: The vaginal walls become thinner and more fragile.
•Drying: The natural moisture and lubrication decrease dramatically.
•Elasticity Loss: The tissue loses its ability to stretch and contract comfortably.
•pH Shift: The vaginal environment becomes less acidic, which can lead to frequent urinary tract infections (UTIs) or yeast infections.
The term Genitourinary Syndrome of Menopause (GSM) is often used by doctors because it accurately encompasses both the vaginal and urinary symptoms that often occur together. This condition is progressive, meaning it tends to worsen over time without intervention.
The Role of Movement: Vaginal Atrophy Exercises
While you can’t exercise your way back to high estrogen levels, you can absolutely improve blood flow, muscle tone, and tissue health, which dramatically mitigates the symptoms of GSM.
1. Pelvic Floor Exercises (Kegels)
This is the number one physical therapy tool for GSM. Many women associate Kegels only with preventing urinary incontinence, but they are crucial for blood flow.
How They Help: Regular Kegel exercises increase blood circulation to the vaginal and vulvar tissues. Increased blood flow is essential for oxygen and nutrient delivery, which helps the tissues maintain some degree of health and elasticity. It also helps improve muscle support and sensation.
The Technique:
Find the right muscles: Imagine you are trying to stop the flow of urine and stop passing gas at the same time. The muscles you tighten are your pelvic floor.
Slow Squeeze: Contract these muscles slowly and hold for 5 to 10 seconds. Relax for the same amount of time. Repeat 10 times.
Quick Flickers: Quickly contract and relax the muscles 10 times.
Goal: Aim for three sets of 10 slow holds and 10 fast flickers, three times a day.
2. Deep Squats and Hip Openers
The health of your vaginal tissue is intrinsically linked to the health and mobility of your entire pelvis.
How They Help: Exercises that open the hips and utilize the deep pelvic muscles, like squats, lunges, and butterfly stretches (Baddha Konasana), improve range of motion and overall circulation to the entire pelvic region. This increased movement helps keep the tissues supple and less prone to tightness and tearing.
Actionable Tip: Incorporate 5-10 deep squats into your daily routine. If you can’t do a full squat, sit on the edge of a sturdy chair and stand up and sit down repeatedly to engage the muscles.
3. Sexual Activity (The Best “Exercise”)
This is often the hardest topic to approach when atrophy causes pain, but it is one of the most effective non-hormonal “treatments.”
How It Helps: Penetration (whether with a partner, dilator, or vibrator) helps to stretch the vaginal walls and prevent shortening and narrowing. Sexual arousal naturally brings blood flow to the genitals (engorgement), which is a crucial mechanism for promoting tissue health and lubrication.
The Mindset: View it as a necessary part of tissue maintenance, like stretching a tight muscle. Consistency is key. This should be done gently, using ample lubrication, and without pain.
Simple, Natural Remedies for Comfort
Movement is essential, but it must be paired with topical solutions to address the dryness and fragility of the tissue.
1. High-Quality Vaginal Moisturizers (Not Just Lubricants)
This is a critical distinction many women miss.
•Moisturizers (Daily Care): These are meant to be used regularly (every 2-3 days), regardless of sexual activity. They cling to the vaginal walls and mimic natural moisture to restore the tissue’s surface water content and normalize pH. Look for products containing ingredients like hyaluronic acid or those specifically formulated for vaginal dryness.
•Lubricants (As Needed): These are used only to reduce friction during intercourse or other activities. Use silicone-based lubricants for sex, as they last longer and provide better slip than water-based ones, which can quickly absorb into atrophied tissue.
2. Plant-Based Oils and Suppositories
Certain natural oils can provide soothing relief and barrier protection to the fragile tissues.
•Coconut Oil: Unrefined, organic coconut oil can be a soothing, gentle moisturizer for the external vulvar area to calm itching and irritation. Note: Avoid placing oil inside the vagina if you are prone to yeast infections, as oils can potentially disrupt the delicate balance.
•Sea Buckthorn Oil: Available in oral capsules, this oil is rich in omega-7 fatty acids. A Swedish study has suggested that oral supplementation with sea buckthorn oil may help improve symptoms of dryness and maintain mucosal integrity in postmenopausal women, though more research is needed. (Source: Journal of Nutrition, 2014)
•Vitamin E Suppositories: Inserting a Vitamin E suppository (or cutting open a capsule and using the oil externally) a few times a week can provide deep moisturization and promote healing of micro-tears.
3. Vaginal Dilators (For Progressive Tightness)
If atrophy has led to significant pain or tightening, leading to painful sex (dyspareunia), dilators offer a progressive, controlled way to gently stretch the tissue.
How They Work: Dilators are smooth, medical-grade tubes of gradually increasing size. They allow you to introduce the concept of penetration back to the tissue at your own pace and consistently prevent the tissue from contracting and shortening. This is often recommended by pelvic floor physical therapists.
Important: Always use these with a generous amount of high-quality lubricant and work with a healthcare professional or physical therapist for guidance.
Taking Action: When to Talk to Your Doctor
While natural remedies are effective for mild to moderate GSM, do not hesitate to speak with a healthcare provider, especially a gynecologist or functional medicine practitioner.
If the pain is significantly affecting your quality of life, your doctor may suggest targeted, highly effective medical options:
Low-Dose Vaginal Estrogen: Applied via creams, rings, or tablets, this is localized estrogen therapy. Because it is applied directly to the affected tissue, very little is absorbed into the bloodstream, making it a safe and highly effective option for most women who cannot or do not wish to take systemic (oral) hormone replacement therapy.
You have the right to a comfortable, pain-free life, regardless of your age or menopausal status. By incorporating consistent movement, using the right moisturizing support, and being brave enough to have an honest conversation with your doctor, you can absolutely restore wellness and comfort. Your body is resilient, and you are worthy of reclaiming your ease.