If you live with Lichen Sclerosus (LS), you know the daily struggle: chronic, intense itching, painful fissures, and the constant fear of scarring and fusion. It can feel relentless, isolating, and often frightening.
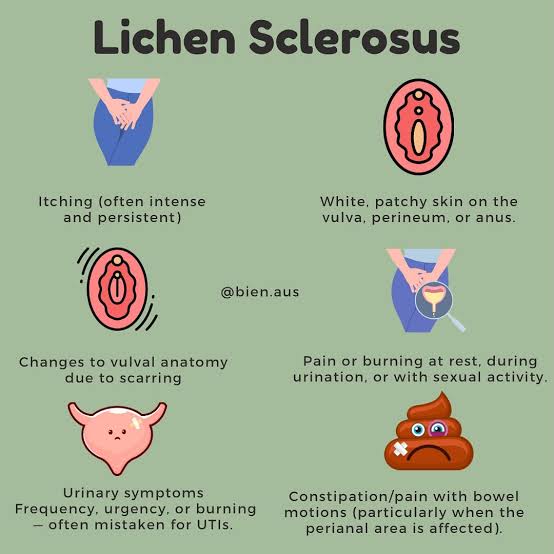
LS is a chronic inflammatory skin condition that primarily affects the skin of the vulva and anus. It causes the skin to become thin, white, and fragile, leading to symptoms like:
- Intense, nocturnal itching (pruritus).
- Easy tearing, bruising, and painful intercourse.
- Progressive scarring and loss of vulvar architecture (fusion).
While the only way to effectively treat the inflammation and prevent scarring is through prescription medication, true long-term relief happens in the home. It requires a committed, daily adjustment to your hygiene, clothing, and moisturizing routine.
Here are the essential steps for long-term management that actually work.
The Non-Negotiable Step: Prescription Steroids
Before discussing at-home remedies, it is absolutely crucial to understand that Lichen Sclerosus cannot be cured by home treatment alone, and not using prescription medicine is dangerous.
Why Steroids Are Essential
The primary and most effective treatment is a high-potency topical steroid (such as Clobetasol or Betamethasone). These are not optional—they are necessary to:
Stop Inflammation: They shut down the chronic inflammatory cascade that causes the severe itching and damage.
Prevent Scarring: They halt the destructive process that leads to fusion and irreversible changes in vulvar anatomy.
Action Plan: Always follow your dermatologist or gynecologist’s instruction for the active treatment phase (usually daily for several weeks) and the maintenance phase (usually 1–3 times per week).
Your Daily Barrier Protection Strategy
Once the inflammation is controlled, the goal is to protect the fragile skin and restore the barrier. This is your core at-home treatment.
1. Daily Barrier Moisturizing (The Golden Rule)
The LS skin is often thin and dry. You must create a protective, occlusive barrier to lock in moisture and protect against friction.
What to use: Use only plain, simple petroleum jelly (like Vaseline) or a thick, unscented mineral oil-based product (like Aquaphor).
When to use: Apply a small amount at least twice a day, and always before exercise, intercourse, or bedtime (when itching is often worst).
2. Ditch All Soap and Wipes
Vulvar skin does not need soap. It disrupts the natural pH and strips away the protective moisture barrier, leading to dryness and irritation.
Rule: Cleanse the area only with lukewarm water, either using your hand or a soft cloth.
Exception: If you feel the need for soap, use only a tiny amount of a non-soap cleanser specifically designed for sensitive skin, and only on the outer thighs/groin, never directly on the vulva.
5 Lifestyle Changes for Long-Term Flare Prevention
The key to LS management is eliminating every source of friction, moisture, and irritation.
3. Change Your Urination Habits
Urine is an irritant. Trapped urine can cause painful burning and inflammation in fragile skin.
Action: Immediately after urinating, gently pat the area completely dry with a soft, dedicated cloth or a damp piece of toilet paper. Apply your barrier moisturizer afterward if needed.
4. Stop All Scratching (The Itch-Scratch Cycle)
Scratching is the enemy of LS. It tears the skin, worsens inflammation, and drives the cycle of itch-pain.
Action: Instead of scratching, apply a small, cool compress or a very thick layer of your protective barrier moisturizer to the itchy area. If nocturnal scratching is an issue, consider wearing soft cotton gloves to bed.
5. Overhaul Your Underwear and Laundry Routine
Friction and chemical residue are major triggers for flares.
Underwear: Wear only 100% white cotton underwear. Avoid synthetic fabrics, thongs, and tight panty lines.
Laundry: Wash your underwear separately in a gentle, fragrance-free, dye-free detergent. Never use fabric softeners or dryer sheets, as the residue is a common irritant.
6. Avoid Prolonged Wetness and Heat
Moisture and heat trap bacteria and friction, increasing irritation.
Action: Immediately change out of wet swimsuits, sweaty workout gear, or damp clothing. Use a soft towel to gently pat the area dry after showering, or use a cool hairdryer on a low setting.
7. Support Your Gut and Inflammation Control (Zinc/Vitamin D)
While not a primary treatment, supporting your overall health can help manage chronic inflammation associated with autoimmune conditions.
Zinc: Involved in skin healing and immune function.
Vitamin D: Deficiency is common and linked to autoimmune activity.
Probiotics: Maintaining a healthy gut microbiome can help regulate systemic inflammation.
Always discuss supplements with your doctor before starting.
Lichen Sclerosus requires daily vigilance, but it is a manageable condition. By consistently applying your medication, protecting your skin barrier, and eliminating friction, you can break the itch-scratch cycle, halt scarring, and reclaim your comfort and quality of life.